This post has been archived and contains information that may be out of date.

The 2025 Behavioral Health Care Symposium is in Sacramento, and it is shaping up to be a great opportunity for behavioral health care professionals.
With a focus on behavioral health policies and best practices, this symposium will bring California’s hospital leaders together to discuss everything from understanding Proposition 1, to measuring trends and outcomes in involuntary treatment, to an in-depth look at building California’s behavioral health infrastructure and its’ historic investments.
Attendees will also learn about Medicaid’s demonstration waiver and inpatient care for individuals with complex needs.
Who should attend?
Health care executives, psychiatric administration and managers, nursing directors, clinical directors, and emergency department staff.
During this holiday season, CHA is partnering with Shriners Children’s Northern California to bring children and young adult books to their patients. Please bring new books to donate during this event.
8:00 – 9:00 a.m. | Check in, Registration, and Continental Breakfast
9:00 – 9:15 a.m. | Opening Comments | Welcome
Kirsten Barlow, Vice President of Policy, California Hospital Association
9:15 – 10:00 a.m. | Opening Keynote | Reflections and Goals for Behavioral Health in California
Maggy Krell, Assemblywoman, District 6
Assemblywoman Krell will share her reflections and goals for behavioral health in California including two behavioral health bills by Assembly Member Krell which were signed into law earlier this month – both were supported by CHA. AB 348 requires counties to prioritize their most vulnerable residents for full-service partnership slots, and AB 416 gives all emergency department physicians a pathway to be county-designated to place and clear involuntary behavioral health “5150” holds.
10:00 – 11:00 a.m. | General Session | HCAI Initiatives: Building California’s Behavioral Health Workforce
Sharmil Shah, MA., Psy.D, Branch Chief, Behavioral Health & Policy, Department of Health Care Access and Information
This session provides a comprehensive overview of the workforce programs and initiatives currently shaping California’s behavioral health landscape. Participants will learn about workforce development opportunities under BH-CONNECT and the Behavioral Health Services Act (Proposition 1), progress being made on the state’s Workforce, Education and Training plan, and broader statewide initiatives aimed at strengthening behavioral health systems.
11:00 a.m. – 12:00 p.m. | General Session | Understanding Prop. 1 of 2024: Public Behavioral Health Reform in Every County
Michelle Baass, Director, Department of Health Care Services
Join Michelle Baass as she discusses Proposition 1 and how it fits into the Department of Health Care Services broader vision and strategy for health care in California. From the Mental Health Services Act to the Behavioral Health Services Act (BHSA), she will share the department’s goals for consumers and families and how hospitals could become involved in the local BHSA planning process.
12:00 – 1:15 p.m. | Hosted Lunch Sponsored by: 
1:15 – 2:15 p.m. | General Session | California’s Efforts to Measure Trends and Outcomes in Involuntary Treatment
Paula Wilhelm, MPP/MPH, Deputy Director, Behavioral Health, California Department of Health Care Services; Janelle Ito-Orille, MA, Chief, Licensing and Certification, Behavioral Health, California Department of Health Care Services; Harris Koenig, President, Harris Koenig & Associates; Megan Barajas, Regional Vice President, Hospital Association of Southern California
State lawmakers passed Senate Bill 929 (Eggman) in 2022 and AB 118 (Budget) in 2023 with an eye toward improving the state’s understanding of how involuntary treatment and conservatorship policies and practices are working in California. Pursuant to these laws, the California Department of Health Care Services recently began collecting and publishing an array of new information about involuntary detentions and conservatorships, but as with any data collection endeavor, it has not been without its challenges. The Department will provide an overview of the phased-in process it is using to collect data from counties and the courts and describe what is being learned so far.
2:15 – 2:45 p.m. | Break and Vendor Visits
2:45 – 3:45 p.m. | General Session | Patients with Acute Behavioral Health Needs: How the BH-CONNECT Demonstration Waiver Can Improve Care
Paula Wilhelm, MPP/MPH, Deputy Director, Behavioral Health, California Department of Health Care Services
The BH-CONNECT initiative seeks to transform California’s behavioral health delivery system by expanding access to highly effective community-based services, strengthening the behavioral health workforce, and ensuring Medi-Cal members receive high-quality care. This presentation will provide a broad overview of BH-CONNECT, as well as highlight several specific components which could improve care for individuals treated in California’s hospitals and health systems.
3:45 – 4:45 p.m. | Building Behavioral Health Infrastructure: A Look at the State’s Historic Investments
Stephanie Welch, Deputy Secretary of Behavioral Health, California Health & Human Services Agency
This presentation provides an overview of California’s nearly $14 billion investment to transform how behavioral health services are delivered and accessed across the state and service continuum – from prevention to long-term care. The presentation will identify how capital infrastructure investments will achieve key goals of the Newsom Administration and California State Legislature: focusing on populations across the lifespan with the highest needs, promoting equity in access to care for people experiencing a primary substance use disorder, addressing whole-person needs such as housing supports, and ensuring accountability.
4:45 – 5:00 p.m. | Pass Through to Reception
5:00 – 6:00 p.m. | Reception
8:00 – 9:00 a.m. | Continental Breakfast
9:00– 9:15 a.m. | Opening Comments | Welcome
Bryan J. Bucklew, FACHE, President & CEO, Hospital Council – Northern California
9:15 – 10:30 a.m. | General Session | Meeting a Growing Challenge: Inpatient Care for Individuals with Complex Needs
Stuart Buttlaire, PhD, MBA, Behavioral Health Consultant and Former Regional Director, Behavioral Health & Addiction Medicine, Kaiser Permanente Northern California; Tandy Burton, RN, MSN, Behavioral Health Director, Woodland Memorial Hospital, Dignity Health, CommonSpirit; Paul Jorge Dizon, MSN, RN, PMH-BC, Senior Clincal Development Nurse 1, GSAA Nursing Professional Development, Kaiser Permanente – Fremont Medical Center: Emily Baldwin, MD, EdM, Medical Director, Behavioral Health Services, Alta Bates Summit Medical Center
This moderated panel explores the design, operations, and financing of medical-psychiatric (med-psych) inpatient units serving adults with co-occurring medical complexity and acute behavioral health needs. Leaders from California programs will share lessons on patient selection, staffing models, throughput, consultation-liaison medicine, and partnerships with EDs, payers, and step-down settings. We’ll translate these lessons to current California realities—staffing, Medi-Cal/Health Plan billing, and post-acute pathways—into practical next steps for hospitals.
10:30 – 11:00 a.m. | Break and Vendor Visits
11:00 a.m. – 12:15 p.m. | General Session | Promoting Peer Respites and the Role of Peers in Inpatient and Emergency Psychiatric Care
Khatera A. Tamplen, Office of Peer Support Services – Manager, Health Equity Division, Alameda County Behavioral Health Department; Jason Robison, Chief Program Officer, The Self-Help and Recovery Exchange; Keris Jän Myrick, MBA, MS, Senior Vice President of Partnerships and Innovation, Inseparable
This presentation equips emergency room and hospital leaders with a clear understanding of peer run respites and peer support services as evidence-based, person-centered services that prevent crisis, reduce avoidable ED utilization/readmissions, and improve patient experience and equity.
12:15 – 1:15 p.m. | Hosted Lunch and Raffle Sponsored by: 
1:15 – 2:15 p.m. | General Session | The Lanterman-Petris-Short (LPS) Act: Myths, Mysteries, and Misunderstandings
Alicia Macklin, JD, MPH, Partner, Hooper Lundy & Bookman P.C.; Linda Garret, JD, Partner, Garrett Law LLP; Mike Phillips, JD, Senior Director of Patient Advocacy and Housing Services, Jewish Family Service of San Diego
This presentation will be a fast-paced, interactive hour focused on separating fact from fiction. What does the law actually say? And what do we think the law says? After decades of trying to match the law to reality, some intriguing myths, mysteries and misunderstandings have established themselves firmly into our common belief system. Prepare to share examples of things you’ve been told are true, “but just can’t prove,” and to disabuse yourself of some things you think are true, “but just aren’t sure.” And, bring some of the odd, unusual or downright nonsensical things you have heard about involuntary holds over the years.
2:15 – 3:15 p.m. | General Session | Early Implementation Experiences of Legal Changes to the Lanterman-Petris-Short Act
Anantha Panyala, PhD, Executive Director, Mental Health Treatment Center, Behavioral Health Services, Department of Health Services, County of Sacramento; Hillary Kunins, MD, MPH, Director of Behavioral Health Services and Mental Health, City and County of San Francisco; James Kwon, Deputy Director, Los Angeles County Department of Mental Health, Office of the Public Guardian; Tony Vartan, LCSW, Founder & CEO, Tony Vartan, LLC, Behavioral Health and Healthcare Consultants
This session will explore the early implementation experiences of California counties and hospitals adapting to recent legal and operational changes to the Lanterman-Petris-Short (LPS) Act, including SB 43 and CARE Court. Panelists will discuss key challenges, emerging best practices, and collaborative strategies for aligning clinical operations, legal mandates, and system capacity in the evolving behavioral health landscape.
- Understand how two new California laws streamline access to behavioral health care patients in need.
- Identify statewide behavioral health workforce initiatives and their impact on service delivery and workforce development.
- Attendees will understand how counties can utilize this funding source as they plan for the future.
- Attendees will gain an understanding of new statewide data reporting requirements, many of which apply to hospitals, for individuals placed on an involuntary hold or conservatorship due to mental illness or a severe substance use disorder.
- Attendees will learn about a major new investment in California’s behavioral health delivery system and ways hospitals can link their eligible patients to new Medi-Cal services and benefits.
- Ability to identify and understand the impact of recent capital infrastructure investments in behavioral health treatment and services capacity across California today and in the coming years.
- Participants will be able to identify at least three operational practices that improve safety, length of stay, and avoidable transfers in med-psych units, and name one metric to track each practice.
- Define current use of Peer Run Respites for individuals with substance use and/or mental health conditions as step-up or step-down services and describe the use of and research supporting peer support services in psychiatric hospital settings.
- Participants will be able to explain three common myths about the LPS Act, and why they are sometimes helpful, but often problematic.
- Participants will be able to identify at least one effective operational or policy strategy for improving care coordination and compliance during implementation of recent LPS Act reforms.
Additional presenters to be added.

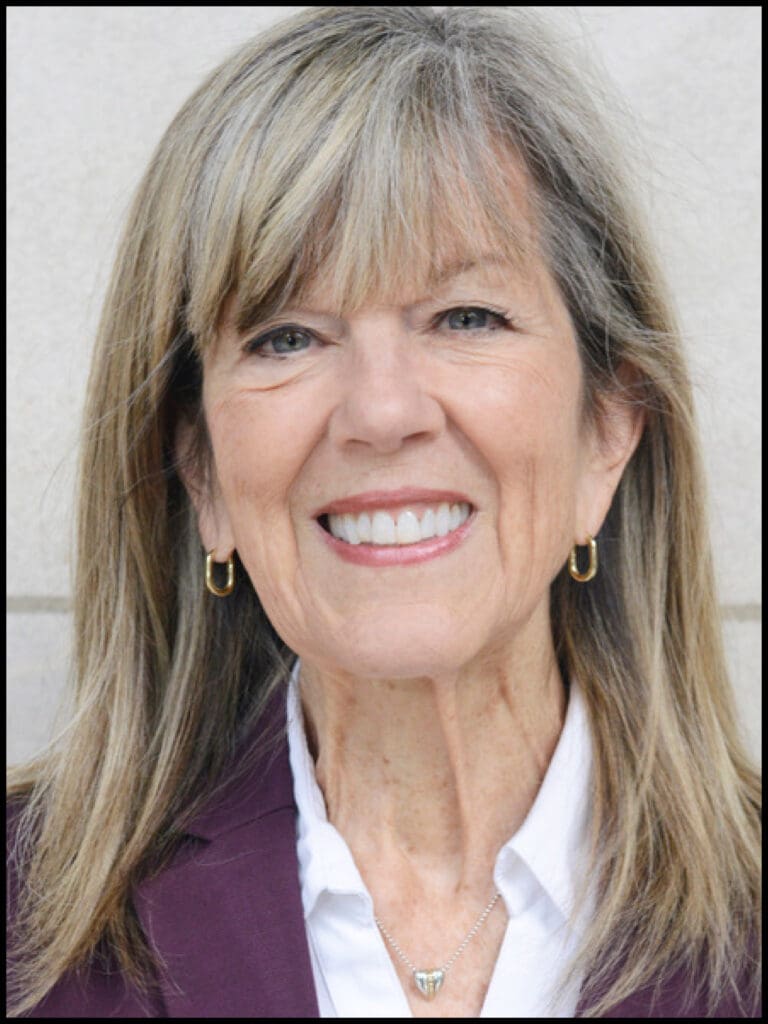
Michelle Baass
Director
California Department of Health Care Services
Michelle Baass was appointed Director of the California Department of Health Care Services (DHCS) in 2021. She leads a team of more than 4,800 individuals at DHCS. Before her appointment to DHCS, Ms. Baass served as Undersecretary of the California Health and Human Services Agency (CalHHS) since 2018 and Deputy Secretary of the Office of Program and Fiscal Affairs at CalHHS from 2017 to 2018. Prior to joining CalHHS, she worked for the California Legislature for 13 years, including in positions at the Senate Committee on Budget and Fiscal Review, Senate Office of Research, and Legislative Analyst’s Office.

Emily Baldwin, MD, EdM
Medical Director, Behavioral Health Services
Alta Bates Summit Medical Center
Emily Baldwin, MD, EdM, is Medical Director for the behavioral health service line at Alta Bates Summit Medical Center, and President of Bay Psychiatric Associates. At Alta Bates-Summit she has served in various leadership positions including as Medical Director for Eating Disorders services and Adult Inpatient services. Her clinical work is presently primarily in the Consult-Liaison service at Alta Bates-Summit.

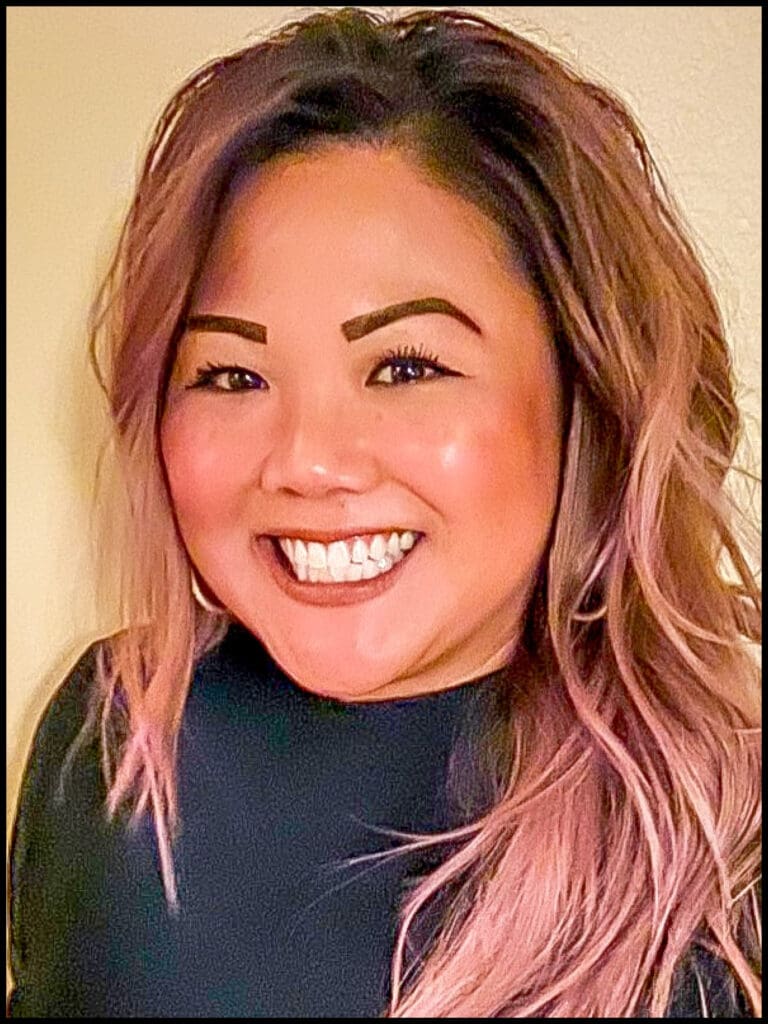
Megan Barajas, MPA
Regional Vice President
Hospital Association of Southern California (HASC)
Megan Barajas represents hospitals across Riverside and San Bernardino counties. She leads regional policy and advocacy efforts on HASC’s strategic priorities, including behavioral health and emergency medical services, and is a key driver behind multi-agency initiatives that strengthen hospital operations and care delivery. She works closely with hospital executives, county departments, managed care plans, and elected officials to advance policies that support access, coordination, and sustainability across the health care system.
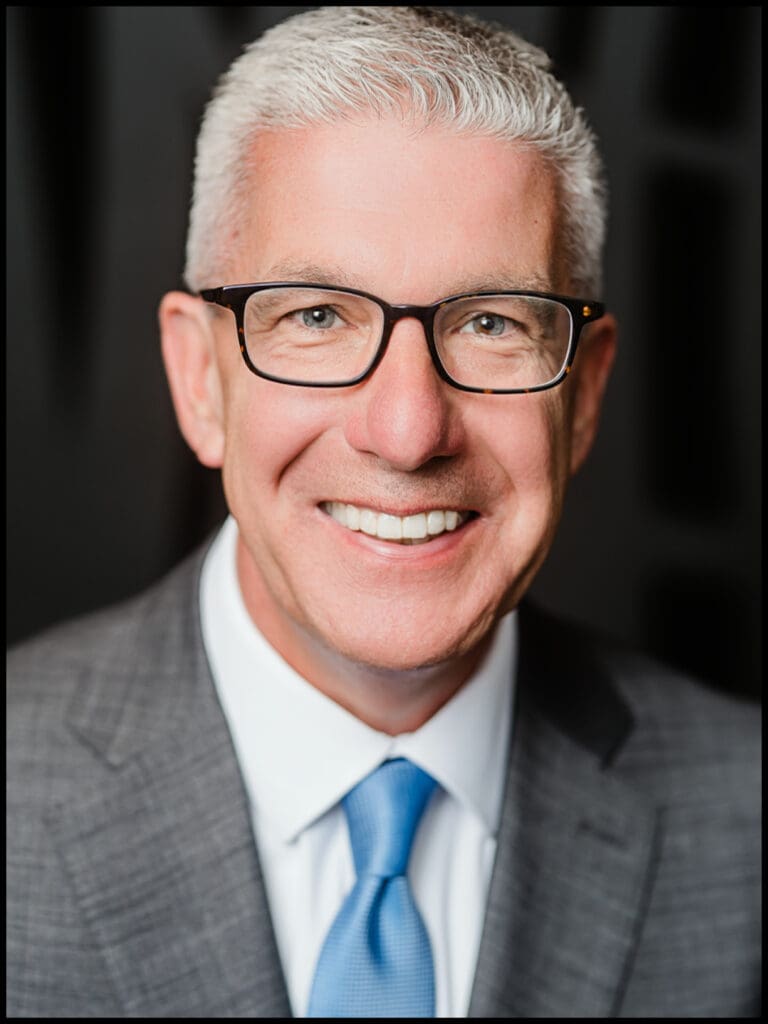
Bryan J. Bucklew, FACHE
President & CEO
Hospital Council – Northern & Central California
Mr. Bucklew leads advocacy efforts on behalf of hospitals and community health. Representing hospitals and healthcare needs of 50 of California’s 58 counties, he works closely with California Hospital Association and its southern association regional partners, the Hospital Association of Southern California and the Hospital Association of San Diego and Imperial Counties.

Tandy Burton, RN, MSN
Behavioral Health Director
Woodland Memorial Hospital
Ms. Burton is the Director of Behavioral Health at Woodland Memorial Hospital with Dignity Health (CommonSpirit Health). Serving behavioral health in Yolo County for the last 10 years, she is committed to making medical care available to patients in psychiatric crisis and has helped positively impact patient care and emergency department throughput in Northern California.

Stuart Buttlaire, PhD, MBA
Retired, Regional Director of Behavioral Health, Inpatient Psych, Continuum of Care and Addiction Medicine
Kaiser Permanente
Dr. Buttlaire is a strategic and innovative leader with a proven record of driving change and advancing healthcare excellence. With over 37 years of experience enhancing clinical quality, implementing strategic innovation, and improving operational efficiency in complex healthcare systems, he is renowned for advancing collaborative care models, integrating behavioral and physical health services, and improving population health outcomes.

Paul Jorge Dizon, MSN, RN, PMH-BC
Senior Clinical Development Nurse 1,
GSAA Nursing Professional Development
Kaiser Permanente – Fremont Medical Center
Paul Jorge Dizon, MSN, RN, PMH-BC, is a Senior Clinical Development Nurse and board-certified psychiatric-mental health nursing leader and educator with 17 years of combined clinical, academic, and leadership experience. He was instrumental in shaping and advancing Kaiser Permanente Fremont’s first Medical-Psychiatric Unit, driving Magnet-aligned excellence through innovative workflows, high-reliability practices, and nursing professional development. As a Caring Science leader and HeartMath® Resilience Instructor, he champions trauma-informed, healing-centered care that strengthens therapeutic connection, staff well-being, and patient outcomes. Paul also leads a collaborative partnership with the National Alliance on Mental Illness (NAMI) to expand community support, improve transitions of care, and reduce avoidable readmissions.
Linda Garrett, JD
Partner
Garrett Law, LLP
Linda Garrett has been providing risk management services to public entity healthcare facilities and providers for over 30 years. She trains healthcare providers on a variety of medical/legal topics including consent, mandated reporting, involuntary mental health treatment, and federal and state medical confidentiality laws. Prior to working as a risk manager, Ms. Garrett practiced as a medical malpractice defense attorney for a law firm in San Francisco, California.
Janelle Ito-Orille, MA
Chief, Licensing and Certification, Behavioral Health
California Department of Health Care Services
Janelle has over 17 years of State of California experience, and is currently serving as the Division Chief of the Licensing and Certification Division for the Department of Health Care Services. In this capacity, she is responsible for engaging with various stakeholders on local issues brought forward by constituents; implementing licensing policy and clinical changes; monitoring budgets and expenditures; and conducting on-site and virtual technical assistance. Prior to this, Janelle served as a Branch Chief for Licensing and Complaints in the Substance Use Disorder Compliance Division. As the Division Chief, Janelle serves as the central point for planning, implementing, and evaluating program policy on all matters related to behavioral health licensing and certification.

Harris F. Koenig
President
Harris Koenig & Associates
Mr. Koenig has broad healthcare experience including strategic development, health care policy, and hospital operations. He served for 20 years as a hospital Chief Executive Officer, the culmination of a 45-year career in healthcare administration. He served as a member of the San Bernardino County COVID response team as the hospital liaison and currently provides support to the County Response Transport and Treatment Executive Group whose goal is improving service to 911 callers. This Group has monitored the implementation of SB 43 and the impact of behavioral health on the RTT system. Mr. Koenig has served as the HASC Inland Empire Board Chair and as a member of the HASC Board of Directors.

Hillary Kunins, MD, MPH
Director, Behavioral Health Services and Mental Health San Francisco
San Francisco Department of Public Health (SFDPH)
During her time with SFDPH, Dr. Kunis has played a part in San Francisco’s significant behavioral health reform, including establishing behavioral health street health teams, an Office of Coordinated Care to have a single point of access to the system of care, and expanding its residential care system by more than 400 beds, including a drug sobering center and crisis stabilization unit. San Francisco has also implemented a coordinated overdose response system, including expanding its treatment network to include, among other initiatives, an evening telehealth program for immediate initiation of medications for addiction treatment.

Maggy Krell
Assemblywoman
District 6
As Deputy Attorney General, Maggy Krell developed a breakthrough legal theory that dismantled the largest on-line sex trafficking operation in the nation. She received a career achievement award from the National Center for Missing & Exploited Children for her work helping survivors. Maggie Krell brings legal scholarship and policy leadership to the California State Assembly.

James Kwon
Deputy Director
Los Angeles County Department of Mental Health
Mr. Kwon has extensive experience in working with vulnerable populations within California, including serving as a program manager for Clausen House, a non-profit agency dedicated to the empowerment of adults with developmental disabilities in Oakland, a Social Worker at Golden Gate Regional Center in San Francisco, a Supervising Deputy Public Guardian at the County of Santa Clara, and the Chief Deputy Public Guardian at the County of Orange.

Alicia Macklin, JD, MPH
Partner
Hooper Lundy & Bookman P.C.
Ms. Macklin is a trusted advisor to a range of inpatient and outpatient behavioral health care providers, along with hospitals and health systems. She has counseled many of California’s hospitals on unsettled areas of law, with an emphasis on compliance with the Emergency Medical Treatment and Labor Act (EMTALA). Her work with providers includes advising on licensing and accreditation, Medicare and Medi-Cal reimbursement, federal and state privacy and confidentiality requirements, and operational issues. She also helps California providers navigate voluntary and involuntary treatment under the Lanterman-Petris-Short Act (LPS Act).

Keris Jãn Myrick, MBA, MS
Senior Vice President of Partnerships and Innovation
Inseparable
Keris Jãn Myrick brings over twenty years of experience advancing mental health policy and systems change at the local, state, and federal levels. A nationally recognized researcher of peer support services, Keris has helped shape the evidence base for peer roles in crisis care, hospital settings, justice settings and community programs. Her work centers dignity, autonomy, and culturally responsive care.

Anantha Panyala, PhD
Executive Director-Mental Health Treatment Center/Division Manager, Behavioral Health Services
Sacramento County
Dr. Panyala has more than 35 years in the field with 20 plus years working in inpatient psychiatric facility. During those years, she held several leadership positions overseeing crisis stabilization and acute inpatient programs. Working collaboratively with Law Enforcement and other community partners, she implemented several initiatives that focused on reducing behavioral health clients being taken to the Emergency Department. Dr. Panyala is currently working on the State’s new legislative changes to the LPS Act.

Mike Phillips, JD
Senior Director of Patient Advocacy and Housing Services
Jewish Family Service of San Diego
In his role at the Jewish Family Service of San Diego, Mike Phillips provides instruction and training for the behavioral health community, including providing information on due process rights for individuals receiving behavioral health treatment throughout the County of San Diego. He also oversees permanent supportive housing programs throughout the Coachella Valley, and safe parking programs throughout San Diego County. He is currently consulting at the state level on behavioral health reform, including participation in the statewide Behavioral Health Action Coalition, and provides both local and statewide law enforcement training on behavioral health issues.

Jason Robinson
Chief Program Officer
Share!
Jason Robison has worked in non-profit management for over 20 years, focusing on education, recovery, housing and health, and serves nationally as a subject matter expert on Peer Services and Recovery-Oriented practices. SHARE! is a peer-run organization in Los Angeles that operates two client-run Centers, two peer-run respite homes, SHARE! Collaborative Housing, and provides advanced peer specialist training throughout California.

Sharmil Shah, MA, Psy.D
Branch Chief, Behavioral Health and Policy
California Department of Health Care Access and Information
Sharmil Shah is a dynamic and innovative leader serving local and state agencies in both the public and private sectors with more than 20 years of clinical, management, community outreach, and business development experience, and a seasoned professional with a high degree of integrity. Her strengths are in behavioral health, team building, collaboration with a broad spectrum of community partners, public speaking, relationship building, outreach, office administration, marketing, and health program administration involving monitoring, evaluating, and assessing community health programs.

Khatera Tamplen
Consumer Relations Manager, Office of Peer Support Services, Health Equity Division
Alameda County Behavioral Health Department
Ms. Tamplen has over 20 years of community service and deep commitment to recovery-oriented systems, peer leadership, and equitable behavioral health care. She also served as a Public Health Advisor within the Substance Abuse and Mental Health Services Administration (SAMHSA) Office of Recovery, leading high-impact national initiatives aimed at transforming crisis response systems and integrating peer support across the behavioral health continuum. This included overseeing the National Mental Health and Substance Use Peer Respite Initiative, uniting leaders from policy, research, and the peer support community to shape forward-thinking federal strategies.

Tony Vartan, MSW, LCSW
Founder & CEO
Tony Vartan, LLC – Behavioral Health & Healthcare Consultants
Tony Vartan is a senior healthcare executive and consultant with over 37 years of leadership experience spanning behavioral health, hospital administration, and acute medical care. He served as Director of Behavioral Health for both Stanislaus and San Joaquin Counties, managing budgets exceeding $265 million and leading more than 600 staff. Prior to his public-sector leadership, Tony spent 19 years with Tenet Health Systems, holding executive roles including Hospital Administrator of a 67-bed psychiatric hospital and Associate Administrator of a 465-bed acute medical center. Through Tony Vartan, LLC, he advises hospitals, health systems, and counties on behavioral health integration, LPS and EMTALA compliance, and strategic service-line development.

Stephanie Welch
Deputy Secretary of Behavioral Health
California Health and Human Services Agency
Committed professional with 20 years of professional experience in mental health policy analysis and advocacy, program development, management and evaluation, and public and community relations at state and local levels.

Paula Wilhelm
Deputy Director, Behavioral Health
California Department of Health Care Services (DHCS)
Ms. Wilhelm joined DHCS in 2022 as an Assistant Deputy Director for Behavioral Health. She oversees behavioral health licensing, certification, and grant programs, and leads policy development and implementation for an array of Medi-Cal and other behavioral health initiatives.
Tuition
Loyalty Members: $350*
*Exclusive loyalty pricing for this year’s conference is available only to CHA members who attended last year’s event. Enjoy a $100 savings. But hurry – this special offer is limited to the first 25 registrants!
*Loyalty pricing is available June 2 – June 30, 2025
Early Bird Members: $450*
Early Bird Associate Members and Government Entities: $450*
Early Bird Nonmembers: $1,000*
*Early bird pricing expires on November 28, 2025.
Members: $529
Associate Members and Government Entities: $529
Nonmembers: $1,100
Members are CHA member hospitals. Nonmembers are non-hospital health care providers, clinics, and post-acute facilities that serve hospitals. Education programs and publications are a membership benefit and are not available to eligible non-member California hospitals.
Cancellation Policy
A $75 non-refundable processing fee will be retained for each cancellation. Cancellations must be made in writing 7 or more days prior to the scheduled event and emailed to education@calhospital.org. No refunds will be made after these dates. Substitutions are encouraged. In the unlikely event that the program is canceled, refunds will be issued to paid registrants within 30 days.
Confirmations
A confirmation will be sent to all registrants. On-site registrations and any unpaid registrations may be subject to an additional 10% fee.
Special Accommodations
If you require special accommodations pursuant to the American’s with Disabilities Act please call (916) 552-7637.
Photography
CHA will photograph this event. If you prefer not to be photographed, please email CHA at education@calhospital.org.
Quality Assurance/Grievance
The CHA education quality assurance/grievance policy is available upon request by emailing rthomason@calhospital.org. If you have any concerns or dissatisfaction with the quality of a CHA education program, please contact Robyn Thomason, Vice President, Education at (916) 552-7514, or email rthomason@calhospital.org.
Questions?
Contact the Education Department at education@calhospital.org.
Full participation in the program is a prerequisite for receiving professional continuing education (CE) credit. Registrant must complete post-event survey, attest to participation and, when required, provide a professional license number. CE certificates will be emailed approximately three weeks after the program. (Amount of CE offered subject to change.)
Behavioral/Social Work — Behavioral Health Care Symposium course meets the qualifications for up to 10.25 hours of continuing education credit for LMFTs and LCSWs as required by the California Board of Behavioral Sciences. CHA is approved by the California Association of Marriage and Family Therapists to sponsor continuing education for LMFTs and LCSWs. Provider approval number 128427. CHA maintains responsibility for this program/course and its content.
At the conclusion of each day, participants will be able to:
Behavioral Health Care Symposium, Day One:
- Understand how two new California laws streamline access to behavioral health care patients in need.
- Identify statewide behavioral health workforce initiatives and their impact on service delivery and workforce development.
- Understand how counties can utilize this funding source as they plan for the future.
- Gain an understanding of new statewide data reporting requirements, many of which apply to hospitals, for individuals placed on an involuntary hold or conservatorship due to mental illness or a severe substance use disorder.
- Learn about a major new investment in California’s behavioral health delivery system and ways hospitals can link their eligible patients to new Medi-Cal services and benefits.
- Identify and understand the impact of recent capital infrastructure investments in behavioral health treatment and services capacity across California today and in the coming years.
Behavioral Health Care Symposium, Day Two:
- Identify at least three operational practices that improve safety, length of stay, and avoidable transfers in med-psych units, and name one metric to track each practice.
- Define current use of Peer Run Respites for individuals with substance use and/or mental health conditions as step-up or step-down services and describe the use of and research supporting peer support services in psychiatric hospital settings.
- Explain three common myths about the LPS Act, and why they are sometimes helpful, but often problematic.
- Identify at least one effective operational or policy strategy for improving care coordination and compliance during implementation of recent LPS Act reforms.
Compliance — The Compliance Certification Board (CCB)® has approved this event for up to 12.30 live CCB CEUs based on a 50-minute hour. Continuing Education Units are awarded based on individual attendance records. Granting of prior approval in no way constitutes endorsement by CCB of this event content or of the event sponsor.
Health Care Executives — CHA is authorized to award 10.25 hours of pre-approved ACHE Qualified Education credit for this program toward advancement, or recertification, in the American College of Healthcare Executives. Participants in this program who wish to have the continuing education hours applied toward ACHE Qualified Education credit must self-report their participation. To self-report, participants must log into their MyACHE account and select ACHE Qualified Education Credit.
Legal — CHA is a State Bar of California approved MCLE provider. Provider number 1980. This participatory activity has been approved for 10.25 hours of MCLE credit.
Nursing — Provider approved by the California Board of Registered Nursing, Provider Number 11924 for 10.25 contact hours.
The Kimpton Sawyer Hotel
500 J Street
Sacramento, CA 95814
(916) 399-4735
The Kimpton Sawyer Hotel has rooms available at a discounted rate of $269 plus taxes and a $25 guest amenity fee per night. For reservations, call (877) 678-6255 and mention the “Behavioral Health Care Symposium” or book online. Don’t delay; the deadline for discounted sleeping rooms is November 17, 2025.
If you would like to sponsor the Behavioral Health Care Symposium contact Lisa Hartzell at lhartzell@calhospital.org.
The California Hospital Association would like to thank our 2025 Behavioral Health Care Symposium Sponsors!
Platinum Sponsors:


Gold Sponsors:




Silver Sponsors:









Take-One Table:
