What’s happening: DataSuite has issued hospital-specific analyses of the inpatient post-acute care transfer (PACT) adjustment policy. The analysis shows the estimated impact on Medicare inpatient fee-for-service payments, and corresponding Medicare severity diagnosis-related group (MS-DRG) volumes from the inpatient prospective payment system (IPPS) during federal fiscal years 2021-26.
(more…)Inpatient Post-Acute Care Transfer Policy Analysis Shows Impact on FFS Payments
Cal/OSHA Standards Boards to Hold Advisory Committee Meeting on Surgical Smoke
What’s happening: On Jan. 20, the Cal/OSHA Standards Board will hold an advisory committee meeting on occupational exposure to plume (surgical smoke) in health care from 10 a.m. to 4 p.m. (PT) via Zoom.
(more…)CARB to Host Public Hearing on Reporting Rules
What’s happening: On Feb. 26, the California Air Resources Board (CARB) will conduct a public hearing to consider approving adoption of the proposed climate data and financial risk reporting regulations.
(more…)National News Shines Spotlight on Horrors of Insurance Company Denials
Over the weekend, CBS News aired an important and timely segment examining the challenges millions of Americans face in accessing health care services due to insurance companies denying coverage for necessary tests and treatments.
(more…)Prop 35 Advisory Committee Presents Revised 2025-26 Spending Plan at January Meeting
What’s happening: At its Jan. 14 meeting, the Proposition 35 Protect Access to Health Care Act Stakeholder Advisory Committee was presented a revised spending plan for calendar years 2025 and 2026. The spending plan reflects investments supported by managed care organization (MCO) tax proceeds generated from taxes imposed on Medi-Cal managed care plans.
(more…)Issue Brief: Bureaucrat-Run Health Care Isn’t the Solution for California’s High Costs
The Issue
Californians deserve a health care system that meets their needs — and hospitals are committed to building one that is both affordable and accessible.
But the Office of Health Care Affordability (OHCA), the state’s answer to the affordability crisis, is destabilizing access to health care across California by arbitrarily capping hospitals’ resources for patient care at unsustainable levels — 3.5%, or even lower for some hospitals — far below the cost of care.
Currently, California’s hospitals are highly efficient. Despite the state’s high cost of living, per capita health care spending ranks in the middle of the pack nationally (29th highest). But hospital-specific spending is far better, ranking 11 places lower — showing that hospitals are already more efficient than the state’s health care system overall.
Meanwhile, insurance companies are headed in the wrong direction. In 2026, health insurance premiums are going up by double digits — putting pressure on Californians’ budgets and sending a sure sign that something is broken. This comes just after a state report showed insurance companies’ profits went up by more than 20% in 2023, while 40% of hospitals lose money every day caring for patients.
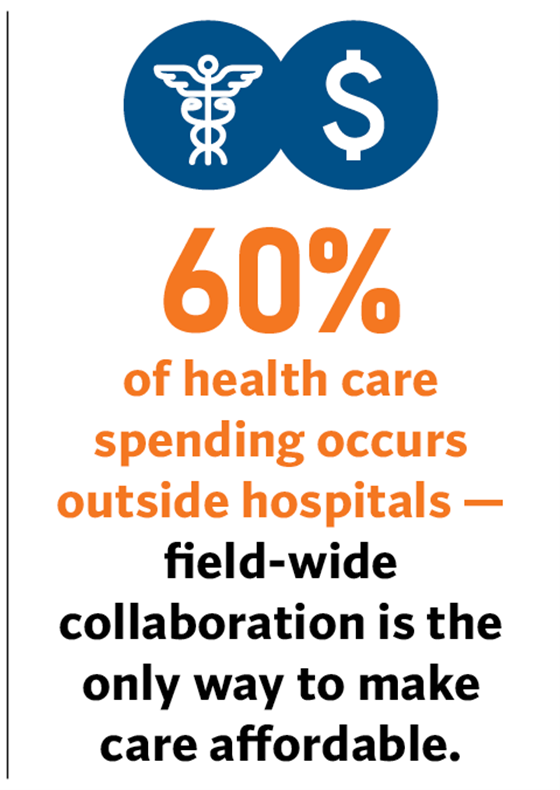
Health insurance companies, drug makers, labor unions, and other stakeholders must work with hospitals and other health care providers to achieve meaningful savings — without collaboration, the consequences for patients will be disastrous.
What’s Needed
Lawmakers must step in to ensure OHCA follows the mandates laid out in statute: improve affordability while maintaining access to and quality of health care.
Hospitals are committed to stopping OHCA’s ill-conceived work before it results in patient harm, and in 2025 CHA filed a lawsuit to challenge whether the board considered threats to access before acting. The lawsuit acknowledges that access to affordable care is a problem across California, and it doesn’t seek to stop OHCA’s work — it simply asks the court to ensure OHCA’s policies comply with its legal obligations to protect health care access and quality.
- Lawmakers can further ensure OHCA’s actions result in lasting, meaningful improvements by:
Supporting legislation that would expand the state’s ability to assess the expected cost, access, safety, and quality impacts of legislation and other policies that place new requirements on health care providers. Ultimately, this would ensure lawmakers have the necessary information to make critical — and sometimes difficult — decisions impacting health care for millions of Californians. - Requiring that OHCA’s spending targets account for the drivers that influence health care costs: economic trends like inflation, legislative mandates, labor costs, changing patient needs, etc.
Key Messages: Bureaucrat-Run Health Care Isn’t the Solution for California’s High Costs
The Office of Health Care Affordability (OHCA) — the state’s response to affordability challenges — is on a path that will debilitate California’s health care system.
(more…)CHA’s ‘Hospital 101’ Briefing for State Legislators and Staff Offers Overview of Hospital Landscape
What’s happening: On Jan. 13, CHA hosted a Hospital 101 briefing to educate more than 60 legislators and legislative staff on hospitals’ role in the health care ecosystem ahead of the new legislative session.
(more…)Resources Available to Support New Mandatory Psychiatric Inpatient Experience Reporting
What’s happening: To support hospitals in reporting Psychiatric Inpatient Experience (PIX) Survey data — mandatory as of Jan. 1 — the Centers for Medicare & Medicaid Services (CMS) has published a host of new resources including data collection templates, a data dictionary, and the Spanish version of the survey.
(more…)HCAI Issues Revised Policy Intent Notice on Emergency Decontamination
What’s happening: The Department of Health Care Access and Information Office of Statewide Hospital Planning and Development (OSHPD) recently revised Policy Intent Notice (PIN) 35 on emergency work authorization for health care decontamination facilities.
(more…)