On Sept. 23, the Department of Health Care Services (DHCS) announced it is updating the Medi-Cal payment system for diagnosis-related group (DRG) reimbursement with the newest ICD-10 diagnosis and surgical procedure codes released by the Centers for Medicare & Medicaid Services, effective for dates of service on or after Oct. 1. However, system updates will not be complete by Oct. 1 and providers who submit claims using the new ICD-10 codes for admission dates on or after Oct. 1 may receive a claim denial until the system update is complete.
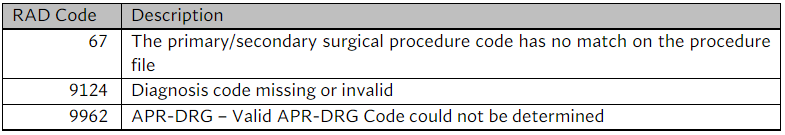
Common claim denial RAD Codes are listed in the table below.
DHCS will not be processing an erroneous payment correction for denied claims related to the Oct. 1 system update. Providers may either hold claims until the system update is complete or may continue to submit claims, but they may be denied. Denied claims can be resubmitted once the system update is complete. DHCS will notify providers via ListSERV notification when the system update has been implemented.
If there are specific questions regarding this update or other DRG-related questions, please contact DHCS at DRG@dhcs.ca.gov.


