Medicare Patient Reclassification Notices Now in Effect
What’s happening: Effective Feb. 14, providers are required to issue a Medicare Change of Status Notice (MCSN) to eligible patients who were admitted as hospital inpatients, but the hospital subsequently reclassified them as outpatients who are receiving observation services.
What else to know: This requirement only applies to patients with traditional Medicare as the primary payer. The form and its instructions are available to download.
(more…)
HCAI Issues Advisory Guide for Building, Remodeling Acute Psychiatric Facilities
What’s happening: The Department of Health Care Access and Information (HCAI) recently released an advisory guide for new construction of acute psychiatric hospitals, psychiatric nursing units provided within general acute care hospitals, and special treatment programs within skilled-nursing facilities — and remodeling or alterations to existing structures of this kind.
What else to know: The advisory guide includes new structural requirements; basic and supplemental services; and mechanical, engineering, and plumbing requirements.
(more…)
Hospital Fee Program Fees Due March 7
What’s happening: Hospital Quality Assurance Fee (HQAF) program 8 fees for the Jan. 1-June 30, 2023, managed care directed payment cycle are due March 7 — and the invoice will be 15% higher than the modeled fee amount.
What else to know: The fee is increased because the Department of Health Care Services (DHCS) is repaying the Centers for Medicare & Medicaid Services (CMS) for inpatient upper payment limit (UPL) overages incurred in HQAF program 6 — and CMS directed DHCS to repay immediately without any flexibility.
(more…)
‘Building the Healthcare Workforce’ Grant Program Proposals Due April 1
What’s happening: To address the chronic health care provider shortage in its counties, the County Medical Services Program (CMSP) Governing Board has released a request for proposals (RFP) for its new Building the Healthcare Workforce (BHW) grant program. The application deadline is April 1 at 3 p.m. (PT).
What else to know: This BHW grant program may support or expand such health care workforce groups as primary care, nursing, behavioral health, dental, allied health, and public health, to name a few. Visit the governing board’s website to download the RFP and associated forms, and submit proposals to grants@cmspcounties.org.
(more…)
Explore Critical Issues Shaping Rural Health Care at 2025 Symposium
What’s happening: On March 10-11 — in less than three weeks — California’s rural hospital industry partners, policymakers, and C-suite health care professionals will gather in Sacramento for CHA’s Rural Health Care Symposium, where they’ll connect on critical issues shaping rural health care.
What else to know: Registration for this two-day event is open to CHA member hospitals.
(more…)
Issue Brief: All Californians Deserve Timely Access to Medical Care
The Issue
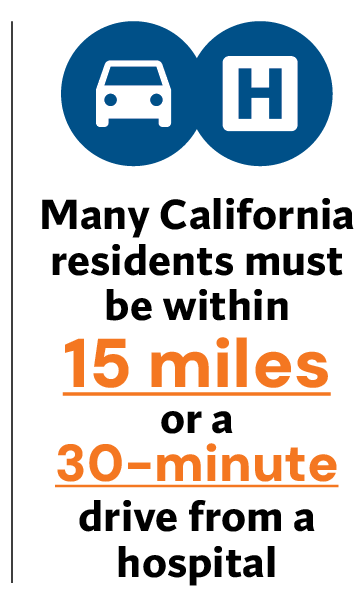
Current California standards require health plans to ensure that their enrollees have timely access to medical care — such as being within 15 miles or a 30-minute drive from a hospital. Unfortunately, many people covered by Medi-Cal still face significant hurdles to access care. This can be addressed by renewing and strengthening these standards to ensure patients have better and more timely access to health care services, including labor and delivery (L&D), behavioral health, and more.
- Without action, California’s standards protecting timely access to care for Medi-Cal enrollees expire on Jan. 1, 2026.
- Every year, Medi-Cal managed care plans can apply for and receive hundreds of exemptions to these standards, and there is no transparency around when or why they are granted.
- Medi-Cal plans are legally required to contract with hospitals treating high numbers of Medi-Cal patients — but the state is not enforcing the contract requirements, putting patients’ ability to access medical care at risk.
- In areas without a hospital L&D unit, an expectant mother who needs to travel as few as six extra miles faces an 11% increase in the likelihood of a negative outcome — yet current law is silent on standards for access to L&D services.
- Current law requires health plans to make outpatient mental health and substance use disorder services accessible to enrollees — within 15 miles or 30 minutes away. However, health plans are not required to make acute behavioral health care services accessible near a person’s home. As a result, people in crisis must often travel several counties away to get the care they need.
For the past eight years, the Legislature has renewed the standards that govern how far and how long a patient must travel for care, but without action in 2025, they will lapse. This could cause millions of patients to lose access to timely and coordinated care. If Medi-Cal patients cannot access in-network providers in the communities where they live, the protections afforded under current “time and distance” standards for health plans are hollow.
What’s Needed
The state must renew, strengthen, and increase enforcement of California’s timely access to medical care standards to help patients relying on health care providers of last resort. Incorporating timely medical access standards for L&D services and acute behavioral health care, whether for inpatient or outpatient services, is critical to reduce the risks of adverse outcomes for expectant mothers and their babies, and to ensure that behavioral health patients receive the care they need in a timely manner.
Key Messages: All Californians Deserve Timely Access to Medical Care
California standards that ensure timely access to care for Medi-Cal enrollees will expire in less than a year.
- These standards require that all health plans ensure their enrollees have timely access to medical care, such as being within 15 miles or a 30-minute drive from a hospital.
- Without renewing these standards, health care deserts across the state could expand.
- Strengthening these standards would ensure patients have better and more timely access to health care services, including labor and delivery (L&D), behavioral health, and more.
The framework for these standards needs increased transparency and oversight to ensure all is being done to protect patients.
- Every year, the Department of Health Care Services (DHCS) provides hundreds of exemptions to health plans’ timely access standards, leaving vulnerable Californians with no other option but to travel — sometimes hundreds of miles — for medically necessary care.
- Unfortunately, the current process provides no assurance that health plans receiving exemptions have exhausted all reasonable efforts to ensure providers are available to treat patients.
- Requiring public reporting of the number of alternative access applications that health plans submit — and how many DHCS approves — would not only shed light on health plans’ efforts to ensure care is there when patients need it, but also build public trust in laws intended to protect patients.
Contracting provisions for hospitals with high numbers of Medi-Cal and uninsured patients should be strengthened.
- Medi-Cal plans are legally required to contract with hospitals treating the most vulnerable patients — but the state is not enforcing the contract requirements, putting patients’ ability to access medical care at risk.
- Patients needing emergency care can visit a nearby hospital, but if their health plans don’t offer contracts to regional hospitals, people needing primary or specialty care must travel a great distance.
Timely access standards for hospital L&D units, as well as inpatient and outpatient behavioral health care services, should be incorporated into state law.
- Incorporating timely access standards for L&D services lowers the risks of adverse outcomes for expectant mothers and their babies, while incorporating such standards for all levels of behavioral health care means better care for patients, which results in better health outcomes.
- There are currently no time and distance standards specific to L&D access. Without these protections, health plans may exclude L&D providers from their network, and patients needing care could be forced to go out of network or travel long distances to access in-network L&D services for delivery.
- Currently, health plans must make outpatient mental health and substance use disorder care available to enrollees within 15 miles or 30 minutes away. However, there are no requirements for inpatient or residential behavioral health care, so people in crisis must often travel several counties away to get the care they need.
New Analysis Shares Potential Impact of FFY 2026 Value-Based Purchasing Program (Third Quarter 2024 Data Update)
What’s happening: CHA DataSuite issued a hospital-specific analysis of the Value-Based Purchasing (VBP) Program, which is based on the most recent publicly available data and program rules established by Centers for Medicare & Medicaid Services (CMS). The analysis is intended to give hospitals a preview of the potential impact of the federal fiscal year (FFY) 2026 VBP program.
What else to know: Comparison to the FFY 2025 program performance is limited as CMS has not yet made final measure and domain level scores available.
Beginning FFY 2026, hospitals will be awarded health equity adjustment (HEA) bonus points for excellent care of underserved populations based on their performance in the four evaluated domains, as well as their percentage of full-dually-eligible patients. An HEA estimate is included in this analysis. There will be winners and losers due to the HEA, as the program slope changes with the additional bonus points.
(more…)
Participant User Guide Assists Hospitals That Signed State’s Data Sharing Agreement
What’s happening: The Center for Data Insights and Innovation (CDII) has released a Participant User Guide for hospitals that have signed the California Data Exchange Framework’s (Dxf) Data Sharing Agreement. The guide explains the information exchange process of health and social services information and outlines how requests for information between Dxf participants — including admission, discharge, and transfer notifications — should occur.
What else to know: CDII also released version 1.2 of the DxF Policy and Procedure “Data Elements to be Exchanged” document, which aligns the state requirement for exchanging health and social services information with the U.S. Core Data for Interoperability information required by the federal Office of the National Coordinator beginning Jan. 1, 2026. The same DxF Policy and Procedure version 1.1 document remains effective through Dec. 31.
(more…)
Correction Requests for Medicare Hospital FFY 2026 Wage Index, Occupational Mix Revised Data Due Feb. 18
What’s happening: CHA DataSuite issued a hospital-specific analysis of the Medicare hospital federal fiscal year (FFY) 2026 wage index and occupational mix revised data — and it is imperative that hospitals review these data, as they have until Feb. 18 to submit requests for either error corrections or revisions.
What else to know: The data analyzed is revised and is the second of three wage and occupational mix data public use files (PUFs) that the Centers for Medicare & Medicaid Services (CMS) issued to develop the hospital wage index for FFY 2026.
(more…)