On Dec. 29, President Joe Biden signed the Consolidated Appropriations Act of 2023, which makes two major changes to COVID-19 pandemic-related Medicaid policies that will have significant impacts on California’s hospitals.
Previous COVID-19-related federal legislation made state Medicaid programs eligible to receive a 6.2 percentage-point increase in the federal government’s share of cost, provided states met certain conditions. (In Medi-Cal, California’s Medicaid program, the federal share of cost is normally 50%.) Among these conditions is the “continuous coverage requirement,” a prohibition against states terminating beneficiaries’ Medicaid eligibility except in limited circumstances, such as those where the beneficiary moves out of state or is deceased. Under this prior law, the enhanced federal funding and the continuous coverage requirement would remain in place until on or after the COVID-19 public health emergency expires, which is not expected to occur until mid-April 2023 at the earliest.
The Consolidated Appropriations Act decouples the enhanced federal funding and continuous coverage requirement from the COVID-19 public health emergency and instead establishes fixed dates for winding down these pandemic-related policies. Under this change in law, the continuous coverage requirement will expire on March 31, 2023, triggering the renewal of Medicaid eligibility redeterminations and terminations. This is expected to result in 2 million to 3 million beneficiaries losing Medi-Cal coverage over the next 14 months.
Additionally, the enhanced federal funding will phase down to zero percentage points, according to the following schedule:
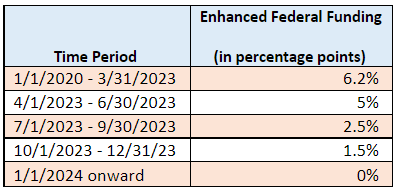
States’ eligibility for the enhanced federal funding after the full enhancement expires on March 31, 2023, is conditional upon state Medicaid programs meeting certain requirements, such as resuming eligibility redeterminations, according to federal rules.
Here’s how the wind-down of these two pandemic-related policies will affect hospitals. First, hospitals may see increases in the number of uninsured patients. Second, given the scheduled reversion of the federal share of the cost to standard levels, the net financial benefit for hospitals will go down in Medi-Cal financing programs where hospitals, rather than the state, pay the nonfederal share of cost.
If you have any questions about these changes in federal law, please contact Ben Johnson at bjohnson@calhospital.org, Robert Ducay at rducay@calhospital.org, or Ryan Witz at rwitz@calhospital.org.



