Office of Health Care Affordability Must Reduce Spending Growth Without Sacrificing Access to Quality Hospital Care
The Issue
The Office of Health Care Affordability (OHCA) has important work ahead as it strives to make health care more affordable for all Californians.
California hospitals stand ready to do their part to slow the rate of growth in health care spending. This work demands equal responsibility from all segments of the health care field — providers, insurers, drug makers, medical device suppliers, labor, governmental agencies, and others.
Making health care more affordable while meeting the needs of 40 million people has never been attempted at this scale. It’s essential that this effort be done with an understanding of the difference between “good” spending (expansion of access to behavioral health care services) and “wasteful” spending (expenditures that add minimal value to improving the health and well-being of Californians).
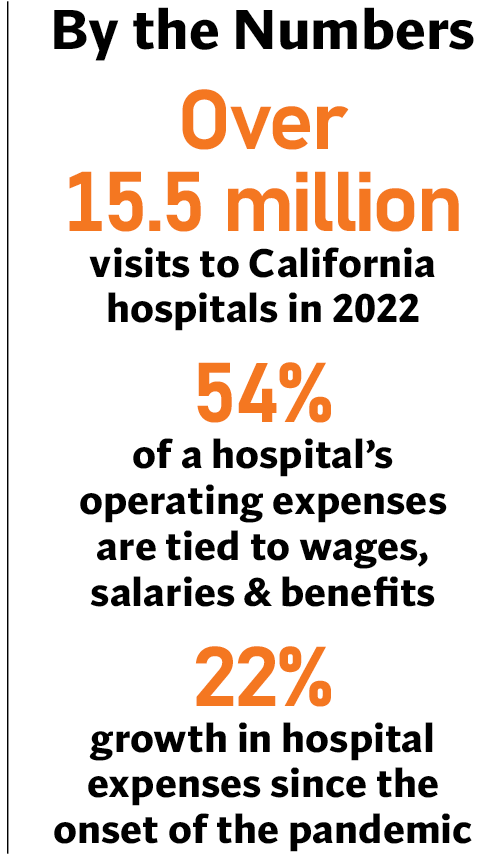
More than 85% of the costs to provide patient care are for items or services hospitals buy from others; these expenses are beyond their control. This includes wages, salaries, and benefits for health care workers, the bulk of hospital expenses. Costs of regulatory requirements — such as California’s seismic compliance mandate — also add significantly to the cost of health care.
California hospitals are working hard to reduce costs and improve affordability through delivery system reform, better care coordination, and clinical efficiencies. When adjusted for the state’s high cost-of-living, California ranks 10th lowest in per capita hospital expenditures in the nation.
What’s Needed
- All-in approach: Every sector of health care must do its part to hold cost growth in check. And governmental payers must recognize that continued underfunding of Medi-Cal and Medicare means commercial insurance premiums and other out-of-pocket costs will continue to increase to cover the shortfall.
- Data-driven decisions: Changes must be informed by data and analysis — not predetermined requirements
such as cost targets that fail to account for the underlying drivers of health care costs. - Improvements to access, quality, and equity: Cost targets should address the rate of growth, not cut
existing health care spending levels, and address underlying deficiencies in the health care delivery system. - Supportive, not punitive, enforcement: Any enforcement processes should be collaborative and responsible.

