Harmful Insurance Company Practices Threaten Patient Care
The Issue
Patients should be able to count on their insurance companies to cover medically necessary, appropriate health care services without delays or improper denials. Yet too many Californians are facing a grave and growing threat to their ability to access critical health care services due to the harmful business practices of many insurers that focus more on the bottom line than on patients.
Access to timely and vital health care services for patients is too often being choked due to practices such as excessive prior authorization mandates, inadequate provider networks, and improperly denied or delayed payments for care provided. These self-serving practices hurt patients and the clinicians who care for them.
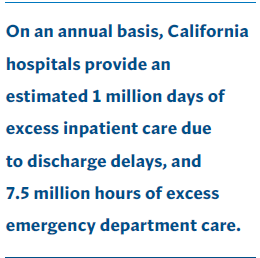
According to a recent survey of California hospitals, 9% of patients — 4,500 people every day — face discharge delays of at least three days after they have been medically cleared for release. Many of these delays are due to insurance barriers. In some extreme cases, patients (especially those experiencing a behavioral health issue) have languished unnecessarily in hospital beds for as long as a year because their insurers do not have adequate provider networks to care for patients after they leave the hospital. Patients enrolled in managed care plans experience these delays at higher rates than those who have fee-forservice coverage such as traditional Medicare.
Care that is delayed is care that is denied. When patients are forced to stay in the hospital longer than necessary, it means medical decisions are being made by insurance companies instead of doctors. It also means worse health outcomes for patients who may need more specialized care.
California has strong laws regulating insurance company practices, but a lack of enforcement has allowed some insurers to avoid their responsibilities. For example, many insurers request reams of paperwork before approving claims, with the hope that hospitals will ultimately give up on trying to receive reimbursement for the care they provided. These ploys result in patients and providers suffering, while insurers profit.
What’s Needed
State regulators must take immediate action to ensure patients get the care they need when they need it. This includes:
- Requiring insurers to pay — in full — the cost of hospital care for patients whose discharge is delayed due
to inadequate post-hospital care networks or prior authorization delays or denials - Directing insurers to specify all reasons for contested or denied claims payments within existing deadlines
- Mandating insurers pay for all care that has been authorized or does not require prior authorization
