Last week, the California Department of Health Care Services (DHCS) announced in a joint statement with five commercial managed care plans (MCPs) that an agreement had been reached on which commercial health plans will serve Medi-Cal patients in 21 counties beginning in January 2024. The agreement relates to the Medi-Cal MCP procurement process that began with a request for proposal (RFP) released on Feb. 9, 2022, and took place throughout 2022.
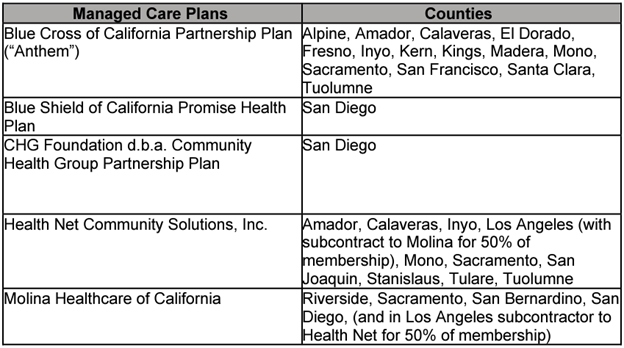
The five MCPs are Blue Cross of California Partnership Plan (“Anthem”); Blue Shield of California Promise Health Plan; CHG Foundation d.b.a. Community Health Group Partnership Plan; Health Net Community Solutions, Inc.; and Molina Healthcare of California.
On Aug. 22, DHCS announced its initial results and intended awardees of the RFP.
These changes to the initial award announcement were based on an agreement reached with the MCPs.
The changes to the original announcement impact Los Angeles, San Diego, and Sacramento counties. Health Net will now serve Sacramento and Los Angeles, but will no longer serve San Diego. Molina maintains San Diego and Sacramento, but will no longer be the primary commercial Medi-Cal plan in Los Angeles. Instead, Health Net will be required to subcontract 50% of its Medi-Cal enrollment to Molina in Los Angeles. Blue Shield and Community Health Group will now also serve San Diego.
The following table lists the new results for the commercial health plans and the counties that they will serve starting in January 2024:
CHA will continue to monitor and communicate updates on the Medi-Cal Managed Care contracting process and subsequent information related to operational readiness requirements.

